Varicose vein sufferers often wonder about whether those unsightly bulging veins put them at risk for other vascular conditions as well.
While many people with varicose veins do not have any other major medical concerns, there may be a higher incidence of conditions like deep vein thrombosis (DVT) when varicose veins are already present. Because deep vein thrombosis is a potentially serious condition if it is left unchecked, it is best to be screened for the disease if you are at higher risk. There are a number of potential risk factors for DVT beyond the appearance of varicose veins that you should be aware of.
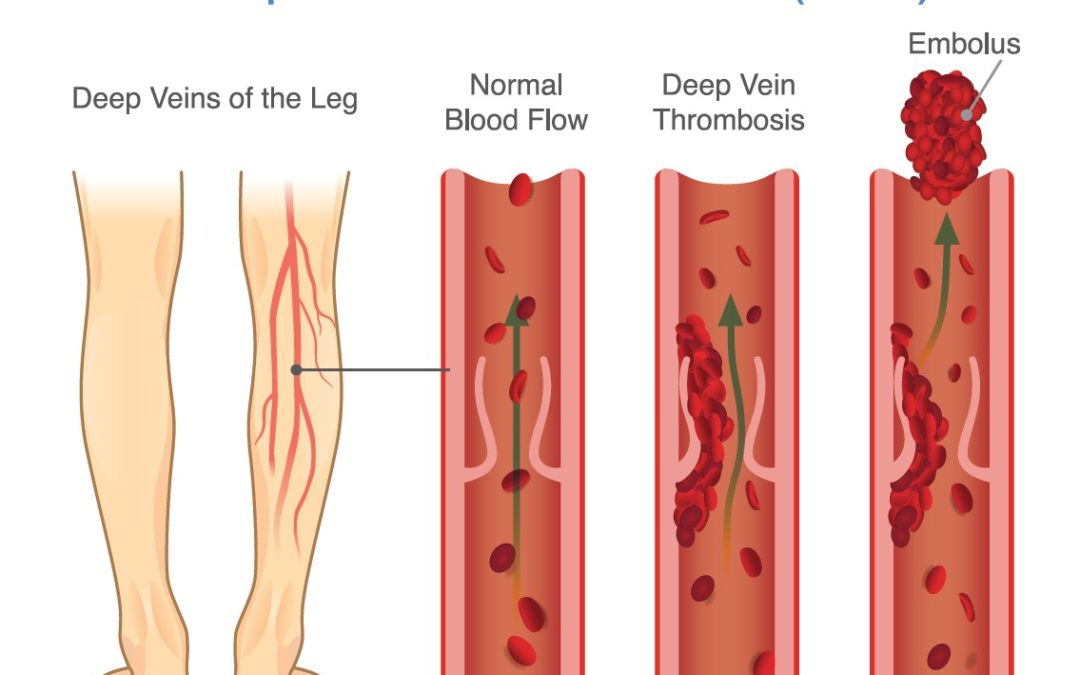
What is DVT?
DVT is a condition in which a blood clot forms in a deep vein of the body, usually the leg. It is a common condition, affecting as many as 600,000 new patients every year. This condition often occurs without symptoms, although some patients may experience pain or swelling in the area of the clot. DVT commonly occurs as a result of blood flow in the area slowing, due to illness, surgery, injury or other inactivity in the leg.
Dangers of DVT
You may not know you have DVT, since many cases do not present with any noticeable symptoms. However, that doesn’t make this condition any less dangerous. The problem is that the blood clot that forms in the lower leg can break free from its initial location at any time without warning. If it does so, the clot can travel through the bloodstream to the lungs, where it can result in a potentially life-threatening event know as a pulmonary embolism.
Symptoms of a pulmonary embolism might include:
• Shortness of breath, difficulty breathing
• Sharp pains in the chest
• Rapid pulse
• Sweating
• Lightheadedness or fainting
• Coughing up blood
If you experience any of these symptoms, emergency medical treatment is needed. Without prompt care, a pulmonary embolism can lead to death.
Risk Factors: DVT can affect both men and women at nearly any age. However, there are some circumstances that increase your risk significantly for this condition. Those factors include:
• Age – While you can develop DVT at any age, it is much more common in adults over the age of 60
• Weight – DVT has been linked to being overweight or obese, a condition that impacts your vascular health overall
• History – If you or someone in your family has a history of a blood-clotting disorder or DVT, your risk factor goes up
• Pregnancy – Women that are pregnant are at higher risk for DVT as the expanding uterus puts additional pressure on the vascular system
• Hormones – Use of birth control pills or hormone replacement therapy can increase your risk for DVT
• Smoking – Nicotine has a negative effect on circulation, which in turn can increase your likelihood of developing DVT
• Medical conditions – Medical conditions like some types of cancer, lupus and inflammatory bowel disease make you more vulnerable to DVT
• Inactivity – DVT risk goes up during long periods of sitting, such as when you are on a long plane ride or an extended car trip
• Bedrest – Spending long periods of time off your feet due to illness, injury or surgery can make you more prone to developing DVT
• Varicose veins – While the jury is still out on how big of a risk factor varicose veins might be in developing DVT, there is a definite correlation between the two
Diagnosing and Treating DVT Because DVT often develops without any noticeable symptoms, the best way to detect the condition is through a diagnostic screening using ultrasound imaging. This painless examination utilizes sound waves to see inside the vessels of the leg, measuring blood flow and detecting any potential problems. Clots can be identified and their location can be pinpointed during this examination, allowing your physician to determine whether you should pursue treatment and the best type of treatment for you.
This test is also used for patients with varicose veins, to diagnose another vein condition known as chronic venous insufficiency or CVI. This condition, characterized by compromised blood flow in the lower leg veins, is often the underlying reason behind the appearance of varicose veins. A proper diagnosis can also help your physician determine which type of vein treatment might be more effective for you.
If DVT is diagnosed, treatment options include medications to dissolve the clot and compression therapy to encourage healthy blood flow in the area. Medications may be taken orally or by intravenous injection, depending on the severity of the condition and how well the patient responds to medication. If medication alone does not dissolve the clot or the patient is unable to take the medication for any reason, a filter may be placed in the large vein of the abdomen, known as the vena cava, to prevent the clot from traveling to the lungs.
The Varicose Veins Connection In addition to varicose veins serving as a possible risk factor for DVT, a patient diagnosed with DVT may be at higher risk for CVI and varicose veins later on. In some cases, the blood clot can weaken the vessel, which allows blood to pool inside the vein. The result is swelling of the vessel and varicosity. CVI can result in uncomfortable symptoms as well as the appearance of varicose veins, such as heaviness or aching in the legs, cramping and swelling of the lower leg and foot.
Varicose Vein Treatment and DVT Like DVT, varicose veins have a number of treatment options today. Nearly all vein treatments are minimally-invasive and require little or no discomfort or downtime. After treatment, you may be prescribed prescription stockings to encourage healthy blood and promote healing in the area. These stockings will also reduce your risk of DVT after your procedure.
Both DVT and varicose veins are conditions that can be effectively diagnosed and treated by a vein specialist. Vein screenings are quick, painless and may help you avoid more serious complications of your condition in the future. To learn more, contact Vein Specialists of the Carolinas at 704-861-2072 or 704-544-5245.