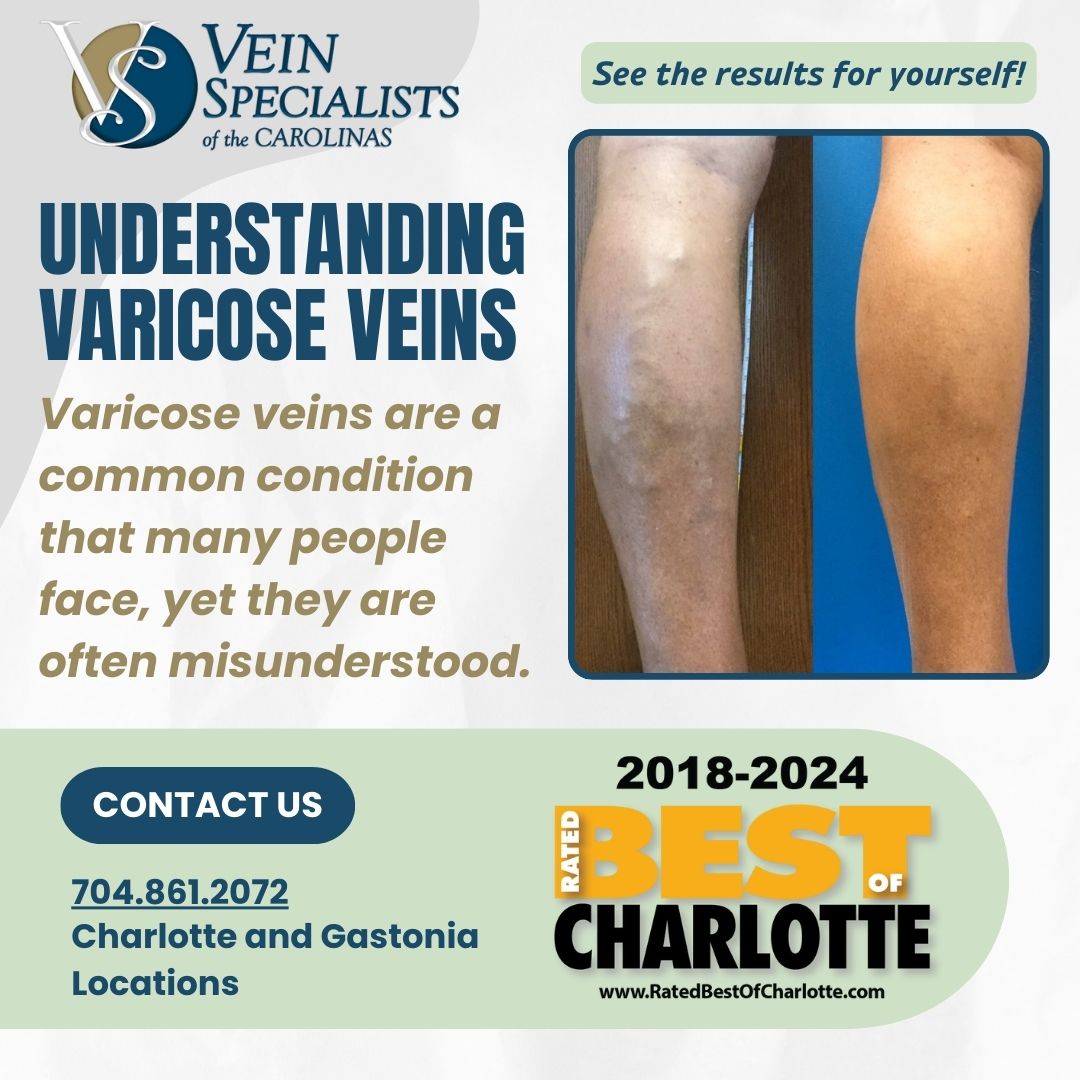
Varicose veins are a common condition that many people face, yet they are often misunderstood.
At Vein Specialists of the Carolinas, we believe that understanding your condition is the first step toward effective treatment. Below are some frequently asked questions about varicose veins and their answers to help you gain a clearer understanding.
What Are Varicose Veins?
Varicose veins are enlarged, twisted veins that often appear blue or dark purple. They typically occur in the legs and are the result of weakened or damaged valves in the veins. These faulty valves cause blood to pool, leading to the bulging appearance of varicose veins.
What Causes Varicose Veins?
Several factors can contribute to the development of varicose veins:
- Genetics: A family history of varicose veins increases your risk.
- Age: The risk increases as you age because veins lose elasticity over time.
- Gender: Women are more likely to develop varicose veins due to hormonal changes during pregnancy, menstruation, or menopause.
- Occupation: Jobs that require prolonged standing or sitting can contribute to varicose veins.
- Lifestyle: Lack of exercise, obesity, and a sedentary lifestyle can exacerbate the condition.
What Are the Symptoms of Varicose Veins?
Common symptoms include:
- Visible, bulging veins
- Swelling in the legs
- A heavy or achy feeling in the legs
- Pain or cramping in the legs
- Itching around the veins
- Skin discoloration around the affected area
How Are Varicose Veins Diagnosed?
Diagnosis typically involves a physical examination by a vein specialist, who will look at your legs while you’re standing to check for swelling. They may also perform an ultrasound to see how your blood is flowing and to rule out any underlying blood clots or other issues.
What Are the Treatment Options for Varicose Veins?
Treatment options range from lifestyle changes to medical procedures, depending on the severity of the condition. Common treatments include:
- Lifestyle Changes: Regular exercise, weight management, elevating your legs, and avoiding long periods of standing or sitting can help alleviate symptoms.
- Compression Stockings: These can help improve blood flow and reduce swelling.
- Sclerotherapy: A minimally invasive procedure where a solution is injected into the vein, causing it to close and eventually fade.
- Laser Treatments: High-intensity laser light can be used to close off smaller varicose veins.
- Endovenous Ablation Therapy: A catheter inserted into the vein uses heat to seal it off.
- Surgical Options: In severe cases, surgery may be required to remove the affected veins.
Are Varicose Veins Dangerous?
While varicose veins are often more of a cosmetic concern, they can lead to more serious health issues if left untreated. Complications can include ulcers, bleeding, and in rare cases, blood clots. It’s important to seek medical advice if you experience significant discomfort or any symptoms of complications.
How Can I Prevent Varicose Veins?
While you can’t completely prevent varicose veins, you can reduce your risk by:
- Exercising regularly
- Maintaining a healthy weight
- Eating a high-fiber, low-salt diet
- Avoiding high heels and tight hosiery
- Elevating your legs
- Changing your sitting or standing position regularly
When Should I See a Vein Doctor?
If your varicose veins cause pain, swelling, heaviness, or if they are causing skin ulcers or other skin problems, it’s time to see a vein specialist. Early intervention can prevent the condition from worsening and reduce the risk of complications.
At Vein Specialists of the Carolinas, we are dedicated to providing comprehensive care for varicose veins. If you have any questions or need a consultation, don’t hesitate to contact us.
For more information, schedule an appointment today!